Follicular lymphoma (FL) is considered an indolent disorder with a relatively favourable course. With modern day treatments, long remissions are often achieved both in front-line and relapsed settings. However, a subset of patients has a more aggressive course and a poorer outcome. Both, PET-CT and minimal residual disease (MRD) evaluation by PCR defines groups of patients with different prognoses. MRD measurement by NGS is being studied to predict relapse prior to diagnostic imaging in large B cell lymphoma; however, it has never been used in FL. The aim of the present study is to validate a sensitive and standardizable approach to measure liquid Biopsy MRD (LiqBio-MRD) by NGS with >90% applicability and 2E-4 resolution, and to analyse its prognostic impact in FL patients.
Firstly, the best source to identify genetic MRD markers was determined. Genomic DNA from paraffin embedded (FFPE) lymph node biopsies and/or cell free DNA (cfDNA) from peripheral blood (PB) was obtained from 29 FL cases at diagnosis and sequenced with a short length Ampliseq Custom Panel (Thermo-Fisher). This panel was designed to cover all coding regions of 56 lymphoma specific genes in FFPE and cfDNA samples. By applying this panel with an average depth of 700X, a total of 122 somatic mutations were detected in 37 baseline samples. 15 of these lymph node samples presented 65 mutations (average of 4 mutations per patient, rank 1-9), with a mean Variant Read Frequency (VRF) of 0.33 (0.06-0.77). On the other hand, the 21 cfDNA samples presented 71 mutations (average of 3 mutations per patient, rank 0-8), with a mean VRF of 0.21 (0.02-1.0). Notably, in 3 cases the mutations were only detected in the lymph node.
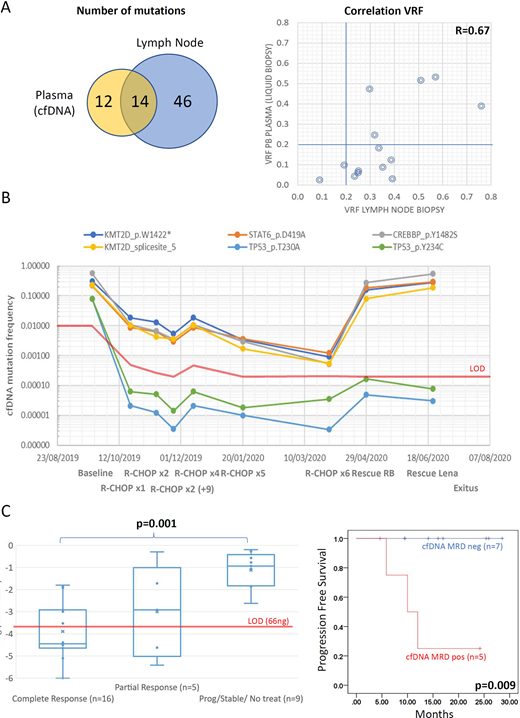
Paired samples were available for 13 cases. Of the 72 somatic mutations identified in these cases, only 14 were present in both samples (Figure 1A, left). Besides the higher number of mutations in the lymph nodes, a mean decrease of 0.14 VRF was observed in cfDNA (0.21; 0.03-0.53) compared to lymph nodes (0.35; 0.09-0.76) (Figure 1A, Right).
From the initial 29 FL cases, 16 had PB sequential samples available. Three patients were put under observation and the rest received an anthracycline based regimen plus R-maintenance. In treated patients, PET-CT was carried out at diagnosis and after 4 and 6 cycles of treatment. During follow-up, cfDNA was available after 4 (n=10) and 6 cycles of treatment (n=10). Median follow up was 18 months. To quantify LiqBio-MRD in the 31 follow-up samples, we defined an approach involving the sequencing of 12 NGS data points per mutation identified at diagnosis. Three of these data points were tumour sample replicates. The other 9 points were obtained from healthy control donor DNA. All LiqBio-MRD samples were sequenced with at least 100.000x and analysed applying the NGS-MRD algorithm described elsewhere (Onecha, E et al. Hematologica 2019). The mean mutation rate (noise) in controls for the studied mutations was 1.4E-5 (0 - 8E-5) below the targeted sensibility of 2E-4. The LOD was defined for every follow-up sample based on the initial amount of cfDNA used in the test. On average 39.6ng (13-66 ng) were used for cfDNA MRD monitoring. All somatic mutations were considered potential MRD markers (Figure 1B), however the degree of MRD in each follow-up sample was defined by the somatic mutation with higher VRF. MRD values were significantly lower in complete response (CR) cases compared to those with active disease (p=0.001, Figure 1C, left). Notably, MRD positivity in the interim or at the end of treatment resulted in significantly inferior PFS (median 12 months vs not reached, P = 0.09, Figure 1C, right). An extension of the cohort and clinical impact of LiqBio-MRD test will be presented at the meeting.
Our results demonstrate for the first time that NGS based MRD quantification is feasible in Liquid Biopsies from FL. Despite the marked spatial genetic heterogeneity of FL, which is better identified in cfDNA, the dilution of the signal in these samples suggests the use of both; lymph node biopsies and cfDNA at diagnosis to identify all potential MRD markers. The lower degree of MRD in CR evaluations (according to the 2014 Lugano response assessment) and the existence of patients in CR with positive and negative MRD suggest the potential of our LiqBio-MRD test to prospectively identify patients with different outcome. Nevertheless, more patients and a longer follow-up are necessary to draw meaningful conclusions.
Heredia:Altum sequencing: Current Employment. Rufian:Altum sequencing: Current Employment. Carrillo:Altum sequencing: Current Employment. Wang:Hosea Precision Medical Technology Co., Ltd: Current Employment. Canales:Janssen: Honoraria; Karyopharm: Honoraria; Celgene: Honoraria; Takeda: Speakers Bureau; Sandoz: Honoraria; Janssen: Speakers Bureau; Novartis: Honoraria; Sandoz: Speakers Bureau; Janssen: Speakers Bureau; Takeda: Speakers Bureau; Roche: Honoraria; iQone: Honoraria; Janssen: Honoraria; Sandoz: Honoraria; Novartis: Honoraria; Roche: Honoraria; Roche: Speakers Bureau; Karyopharm: Honoraria; Gilead: Honoraria; Sandoz: Speakers Bureau; Roche: Speakers Bureau. Martinez-López:Janssen, BMS, Sanofi, Novartis, Incyte, F. Hoffmann-La Roche and Amgen: Honoraria, Other: Advisory boards; Janssen, Novartis, BMS, Incyte: Consultancy; Hosea and Altum: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal